Living WITH back bones - Literally!
Enjoy this special issue on Spine
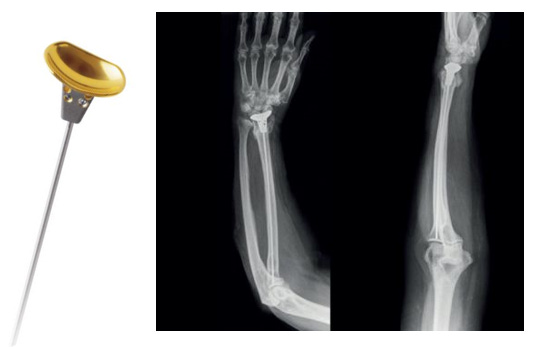
SI joint would like to be loved too… #NeoArmory:
SI joint is like the Spine’s forgotten little child left Home Alone before a big European holiday. Studies estimate SI joint dysfunction can be behind 15-35% of LBAs. Although we are picking this up more recently, we need more modalities of management.

The Catamaran® SI Joint Fusion System from Tenon Medical (CA, USA), aims to address the Kevin Mcallister (Homealone) situation. It is a Robust Titanium peg type implant to transfix and help fuse the SI joint. Uses an inferior-posterior approach and transfixes along a longitudinal axis.

Mechanical testing shows it being a reliable stabilization system and a single centre study concluded a good reduction in SI joint pain.

MAINSAIL study has given out interim 6 month result that suggests 61% pain reduction(VAS), 93% patient satisfaction, No re-operation, No reintervention and 80% success rate.
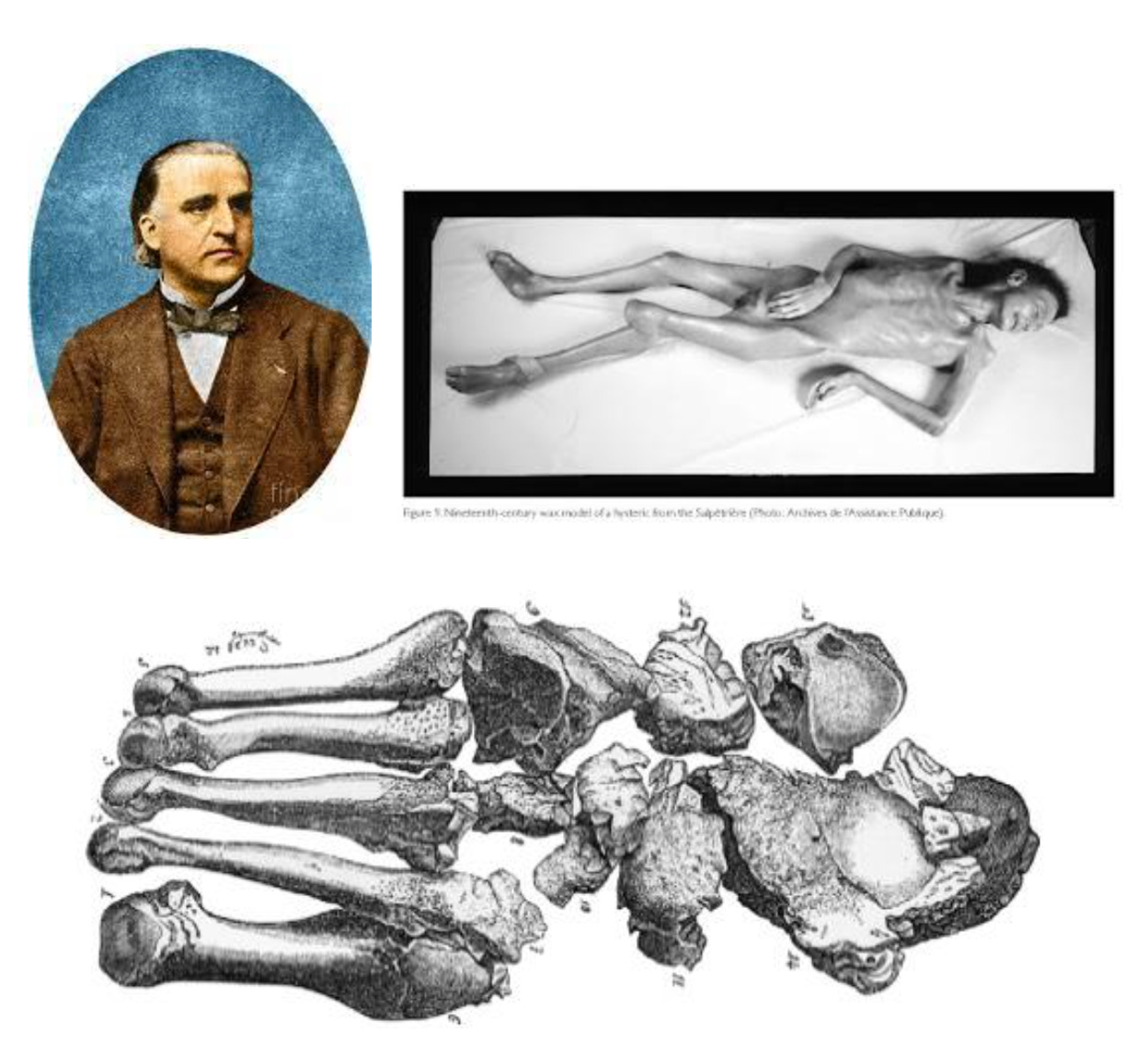
The “Crazy” Surgeon Who Straightened Spines - The Hidden Chapters from Dr. Paul Harrington’s Legacy: #FromTheHistory
Most orthopedic surgeons have heard of the Harrington Rod, the pioneering spinal implant that changed scoliosis treatment and posterior instrumentation forever. But only a few know the backstory of the man behind it - Dr. Paul Randall Harrington, the orthopedic maverick from Kansas who literally built modern spine surgery from scratch.
Back in the 1950s, when polio was leaving children with severe spinal deformities, Harrington wasn’t satisfied with braces and casts. He wanted internal fixation—something unheard of back then. So what did he do? He started crafting metal rods with hooks and ratchets for internal use. Before each surgery, he would hand-fashion the instruments himself—and after each case, he’d tweak the design based on what worked or didn’t. It was surgical innovation in real-time, one patient at a time. But the medical community wasn’t impressed at first. In 1958, when he presented his technique at the AAOS meeting, he was met with “astonishment and deep skepticism. Some even wanted him expelled from the society. He was denied residents, sidelined by colleagues, and nearly booted from his local medical society after early failures. They called him a “crazy man.” He kept going anyway.
Eventually, he convinced the society with his results and partnered with Zimmer Inc. to manufacture the rods - but only allowed sales to surgeons who had personally trained under him. For the first two years, no one could buy a Harrington rod without seeing it in action first. He believed patient safety and proper training were non-negotiable. And those royalties? Until 1970, he donated every cent—$0.50 per rod, $0.25 per hook—to research. Only later, when peripheral vascular disease limited his mobility, did he accept payment.
From basement tinkering to global impact, Dr. Harrington’s legacy is more than metal. It’s about grit, guts, and the belief that a single surgeon, even a ridiculed one, can reshape medicine.

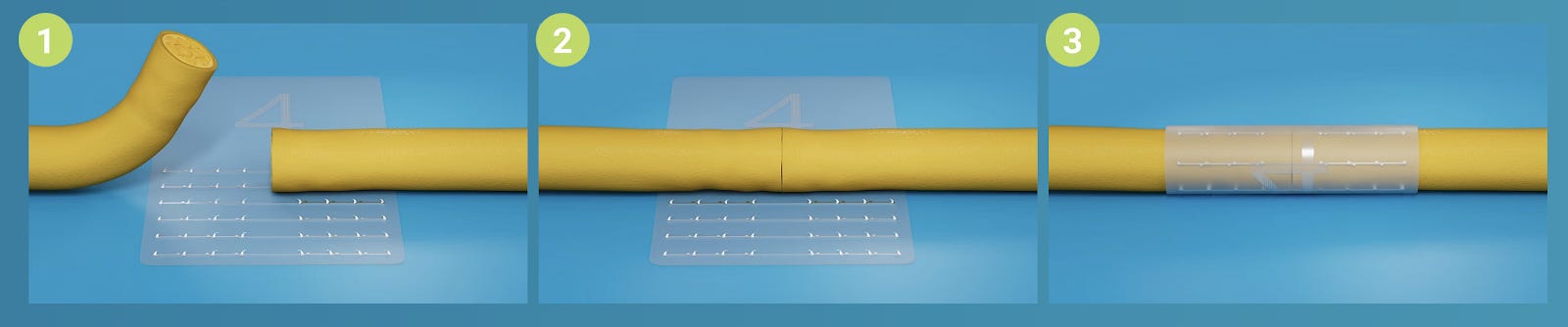
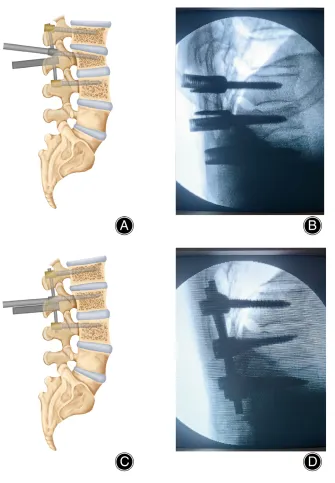
Leverage Technique Using Monoaxial Pedicle Screws for Thoracolumbar Compression Fractures #SurgicalPearl
#SurgicalPearl:
This technique by Zhu et al. enables direct vertebral body reduction by leveraging monoaxial screws, minimizing distraction-related complications such as screw loosening and implant failure. It is particularly effective for AO Type A3 fractures.
Let us provide you with the pearls:
- Posterior midline approach is used to expose the transverse and articular processes of the injured and adjacent vertebrae.
- Monoaxial screws are inserted into the fractured vertebra, parallel to its superior endplate.
- Multiaxial screws are placed in the vertebrae above and below.
- Rods are contoured to match the physiological sagittal profile.
- Rods are seated and caudal nuts are tightened to anchor the rod.
- A rod gripper is locked onto the rod, contacting the inferior edge of the monoaxial screw heads.
- As the monoaxial screw nuts are tightened, the screw tail shifts caudally and the tip elevates cranially.
- This fulcrum-based action lifts the superior endplate of the fractured vertebra.
- Reduction is confirmed when the screw and rod are perpendicular.
- Cranial nuts are then locked without applying distraction. C-arm fluoroscopy confirms reduction and hardware positioning.

Should we operate discs early #InTrials:
Mutubuki et al conducted an RCT and an economic analysis that followed 72 adults who were stuck on a waiting list for surgery for lumbar herniated discs. The researchers randomly divided them into two groups: one got the traditional care approach, while the other received a two-pronged strategy combining Mechanical Diagnosis & Treatment (MDT, a targeted exercise-based therapy) alongside a transforaminal epidural steroid injection (TESI). Over a year, the combo group showed impressive results: vastly fewer of those patients ended up needing surgery, and they saved around €1,700–€2,300 per person, depending on whether you’re looking at healthcare costs or broader societal costs. In short, this combo intervention didn’t just ease pain and avoid surgery—it also made serious economic sense.

It’s the kind of study that might change how we tackle lumbar disc issues, especially when surgical resources are tight or patients prefer to skip cutting altogether.
Don’t forget to check the full study!
Restoring the Curve: Segmental Lordosis and Its Ripple Effect on Adjacent Segment Disease: #MostCited:
Restoring alignment is an important consideration in spinal fusions. Failure to correct to level-specific alignment goals could promote the development of adjacent segment disease (ASD). Singh et al. explored the consequences of inadequate L4–S1 lordosis correction during short lumbar fusions. The findings are sobering: failure to restore segmental alignment within the optimal 35°–45° range significantly increases the risk of ASD and revision surgery within two years.
Among 168 patients with 1–3 level TLIF and two-year follow-up, 32.7% developed ASD and 19.6% required revision. When stratified by adequacy of L4–S1 lordosis restoration, those with optimal correction had markedly lower ASD (6.7% vs. 33.3%) and revision (5.7% vs. 25.9%) rates. Notably, ASD patients had higher implant-related complications (36.8% vs. 8.0%) and were more likely to undergo subsequent revision (61.1% vs. 8.7%).
Hence, sagittal alignment isn’t just aesthetic—it’s biomechanical insurance. In degenerative spine fusion, restoring segmental lordosis may be the difference between durable outcomes and downstream complications
Events to check out:
-
IMAST 2026 – International Meeting on Advanced Spine Techniques 15 – 17 April 2026 Toronto, Canada
-
EFORT Annual Congress 2026 04 – 06 May 2026 Malaga, Spain
-
BioSpine 9 20 – 22 May 2026 Berlin, Germany
Have A fabulous month ahead folks!